Pancreatic cancer, a formidable adversary in the realm of oncology, has established itself as a significant global health concern. In 2020 alone, the diagnosis of this disease afflicted over 495,000 adults worldwide, solidifying its position as the 12th most prevalent cancer globally. Particularly daunting is its impact in the United States, where it stands as the fourth leading cause of cancer-related deaths. Amidst these staggering statistics, pancreatic ductal adenocarcinoma emerges as the predominant villain, constituting approximately 90% of all cases, yet boasting a disheartening average 5-year survival rate of less than 10%. Despite the strides made in cancer therapy, traditional treatments like chemotherapy have failed to significantly enhance survival rates for this aggressive cancer variant.
Underpinning the pathology of pancreatic cancer lies a genetic culprit: mutations in the KRAS gene. More than 90% of pancreatic cancer patients exhibit mutations in their KRAS genes, pivotal players in regulating cellular growth and death. However, recent research from The University of Texas MD Anderson Cancer Center offers a glimmer of hope amidst this bleak landscape. Their study, published in the journal NPJ Precision Oncology, unveils a potential lifeline for patients harboring specific KRAS mutations, hinting at improved survival rates.
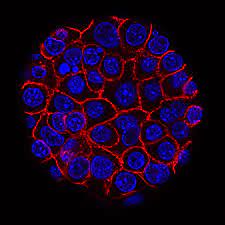
Dr. Dan Zhao, co-lead author of the study, sheds light on the diagnostic and therapeutic intricacies of pancreatic cancer. Situated behind the stomach, the pancreas, a vital component of the digestive system, secretes enzymes crucial for food digestion and regulates blood sugar levels through insulin production. Despite its pivotal role, pancreatic cancer often evades early detection due to the absence of symptoms, leading to challenges in timely intervention. Treatment modalities vary depending on the cancer’s stage, with surgery remaining an option for localized disease. However, as the cancer progresses, conventional therapies falter, necessitating the exploration of novel treatment avenues.
Central to the quest for effective pancreatic cancer therapy is understanding the role of KRAS mutations in cancer pathogenesis. Dr. Zhao elucidates the oncogenic potential of KRAS mutations, underscoring their ability to drive aberrant cellular proliferation and metastasis. Notably, the study identifies distinct survival outcomes associated with different KRAS mutation subtypes, with KRAS G12R mutations offering a glimmer of optimism for improved prognosis.
The emergence of targeted therapies, such as KRAS G12C inhibitors, marks a significant stride in combating KRAS-mutated cancers. While these inhibitors have garnered FDA approval for lung cancer treatment, their efficacy in pancreatic cancer remains under investigation. Dr. Zhao’s ongoing clinical trial aims to shed light on the safety and efficacy of Adagrasib monotherapy in pancreatic ductal adenocarcinoma, offering a beacon of hope for patients in dire need of effective treatment options.
Beyond targeted therapies, the tantalizing prospect of a cancer vaccine looms on the horizon. The KRAS G12C inhibitor paves the way for vaccine development, with phase 1 clinical trials showing promising results in colorectal and pancreatic cancers. Dr. Anton Bilchik, a surgical oncologist, emphasizes the significance of vaccine therapy in combating pancreatic cancer, underscoring its potential to revolutionize treatment paradigms.
In essence, while pancreatic cancer continues to pose formidable challenges, recent advancements in understanding its molecular underpinnings offer a glimmer of hope. The quest for effective therapies, whether through targeted inhibitors or innovative vaccine strategies, signifies a united front in the battle against this relentless disease. As researchers and clinicians forge ahead, fueled by optimism and determination, the prospect of transforming pancreatic cancer from a grim diagnosis to a manageable condition beckons on the horizon.